Teaching complementary and alternative medicine in undergraduate medical education: a scoping review
Mary Soliman and Justin Bilszta
Department of Medical Education, Melbourne Medical School, University of Melbourne, Australia
Submitted: 27/11/2020; Accepted: 05/07/2021; Published: 27/07/2021
Int J Med Educ. 2021; 12:140-149; doi: 10.5116/ijme.60e2.f3ed
© 2021 Mary Soliman & Justin Bilszta. This is an Open Access article distributed under the terms of the Creative Commons Attribution License which permits unrestricted use of work provided the original work is properly cited. http://creativecommons.org/licenses/by/3.0
Abstract
Objectives: This scoping review explores the extent to which undergraduate medical education have incorporated complementary and alternative medicine in their curricula and evaluates the teaching, delivery and assessment approaches used.
Methods: ERIC, Ovid Medline and Pubmed databases were searched with keywords related to “complementary and alternative medicine” and “undergraduate medical education” for relevant articles published until August 2020. Data extraction included the presence/absence of complementary and alternative medicine integration, program duration, instructor background, and assessment methods.
Results: Of 1146 citations, 26 met the inclusion criteria. Complementary and alternative medicine teaching in undergraduate medical education was widely inconsistent and not well aligned with clearly identified aims and objectives. Various complementary and alternative medicine disciplines were taught, demonstrated or observed, and several programs included teaching on evidence-based medicine. Educational outcomes mainly assessed student satisfaction and learning through self-evaluation and rarely assessed for effectiveness with regards to changing clinical practice or impacts on patient outcomes.
Conclusions: Inconsistencies in complementary and alternative medicine teaching and assessment in undergraduate medical education reflect the lack of defined graduate competencies. An evidence-based medicine component of an educational program is a potential solution to overcoming breadth and content challenges. Curriculum developers would be better guided with research that determines if complementary and alternative medicine program design, content and assessment influence clinical practice and/or patient outcomes.
Introduction
Medical educators encounter various challenges incorporating complementary and alternative medicine (CAM) teaching into undergraduate medical education (UGME). The term CAM relates to the use of non-mainstream practices, either together with conventional medicine (complementary), or in place of it (alternative).1 Common complementary health approaches include the broad descriptors of natural products (herbs, vitamins, minerals, probiotics), and mind and body practices (yoga, chiropractic, osteopathic manipulation, meditation, acupuncture, breathing exercises). In addition to the enormous breadth of CAM, there exists a degree of uncertainty around the validity and efficacy of many widely used therapies.2 Whereas conventional western medicine defines ‘best practice’ based on empirical trials utilising large patient populations, many CAM therapies boast an individualised approach where the practitioner-patient interaction is therapeutic rather than the therapy itself.2 This poses a considerable challenge for educators tasked with determining the necessary acquisition of CAM knowledge and skills in UGME.
Despite a need to upskill medical students in CAM-related knowledge and practice, there has not been an authoritative consensus regarding the acquisition of CAM skills and knowledge in medical students at graduation or the optimal method to provide this education. This raises the question as to what evidence and scholarship can curriculum developers draw upon to plan and implement CAM curricula for UGME students? A preliminary search of the literature, whilst failing to identify any reviews which have systematically investigated CAM teaching in UGME curricula, did provide some insight into the challenges (and innovations) medical schools face in teaching and assessing student learning related to CAM practices. Stratton and Colleagues (2007) surveyed CAM educational programs funded by the National Center for Complementary and Alternative Medicine (NCCAM). They found an array of curricula exist to provide health professions students with the necessary knowledge, attitudes, and skills to address CAM-related issues, and the approaches to evaluating curricular efforts were equally diverse; limiting the survey to only those that received NCCAM funding means it is difficult to generalise the findings.3 The second attempted to systematically evaluate evidence of effective CAM educational interventions for both biomedical doctors and medical students.4 This review only focused on descriptions of randomized controlled trials (RCTs), nonrandomized controlled trials (non-RCTs), and before and after studies. Importantly, it did not specifically examine descriptions of integrating CAM materials in the broader context of UGME curricula, nor did it explore the variety of teaching, learning and assessment approaches UGME programs utilise. This latter issue is of particular interest as it is important to determine if there is a correlation between changes in student’s CAM-related attitudes, knowledge, skills and the provision of patient care.
We, therefore, conducted this scoping review of primary studies to evaluate the different approaches UGME programs have taken to incorporate CAM teaching into their curricula and identify directions for future research. The specific research questions we sought to answer were: 1. do UGME programs teach students about CAM and, if so, which CAM disciplines do UGME programs teach students? 2. what teaching and learning approaches do UGME use to teach students about CAM? and; 3. how are UGME students assessed about their knowledge of CAM? In addition to these questions, this review also evaluated the effectiveness of CAM teaching in the included studies, using the Kirkpatrick Hierarchy for Assessing Educational Outcomes.5-7
Methods
This study adopted the “Preferred Reporting Items for Systematic reviews and Meta-Analysis extension for Scoping Reviews” (PRISMA-ScR) reporting protocol.8
Search Strategy
Electronic databases ERIC, Ovid Medline and PubMed were searched for full-text articles describing the delivery of CAM teaching in UGME (see Table 1). Additional papers were found through a hand search of the reference lists of articles identified through the online database search.
Inclusion and Exclusion Criteria
There was no limit on the publication date. Only full-text articles written in English were included. Articles were limited to those that looked exclusively at UGME, with medical students only. Articles exploring medical students’ or faculty members’ attitudes regarding CAM were excluded. Articles that did not clearly describe the characteristics of CAM teaching within the UGME curricula (for example, topics taught in CAM programs, duration or frequency of teaching programs, methods used to assess student learning, etc.) were also excluded, as were general articles about CAM in medical education, and proposals for CAM curricula without implementation and opportunity for subsequent evaluation.
Key terms and Boolean Operators
Complementary and alternative medicine, CAM, complementary medicine or alternative medicine, homeopath*, Chinese medicine, undergraduate medical, medical school, medical education, medical course, medical cirricul*, teach, university.
Data Extraction and Charting
Data extraction was performed using a predetermined list, and included:
· Article details: first author and publication year
· Participant information: student cohort, institution, or country/city of institution
· Information gathering approach: questionnaire, survey, telephone interview
· Educational intervention: presence or absence of CAM integration, topics taught in CAM programs
· Duration or frequency: time spent delivering teaching within the program
· Instructors background: qualifications or title of educators
· Outcome assessment: methods used to assess program aims, primarily students’ qualitative and quantitative course evaluation
· Educational outcome: assessed using Kirkpatrick’s Hierarchy of Educational Outcomes, a well-recognised tool for the evaluation of the effectiveness of medical, educational outcomes.5-7 The bottom level assesses learners' satisfaction with, or reaction to, the Intervention; the second level assesses modification of students’ attitudes and perceptions and/or the knowledge and skills learned; the third level assesses changes in health professionals' behaviour or an institution's practice, and; at the top of the hierarchy, changes in patient health care outcomes. In this review, Kirkpatrick’s Hierarchy was used to assess educational interventions as they relate to specific CAM programs taught within UGME curricula.
Limitations: identified program limitations
Synthesis of Results
Each of the included studies was described by the author, year of publication, and the characteristics listed above. Thematic analysis was conducted to identify commonalities between the included studies. No inferences were made about CAM teaching, learning, and assessment approaches if they were not explicitly stated. Literature searching, title and abstract screening, full-text review and data extraction and charting were undertaken by the first author (MS). Where there was any uncertainty regarding the aforementioned, these articles were reviewed independently by the 2nd author (JB) and then discussed until consensus was reached between both authors. The 2nd author also independently reviewed the data extraction and charting results once this process was completed by the first author.
Results
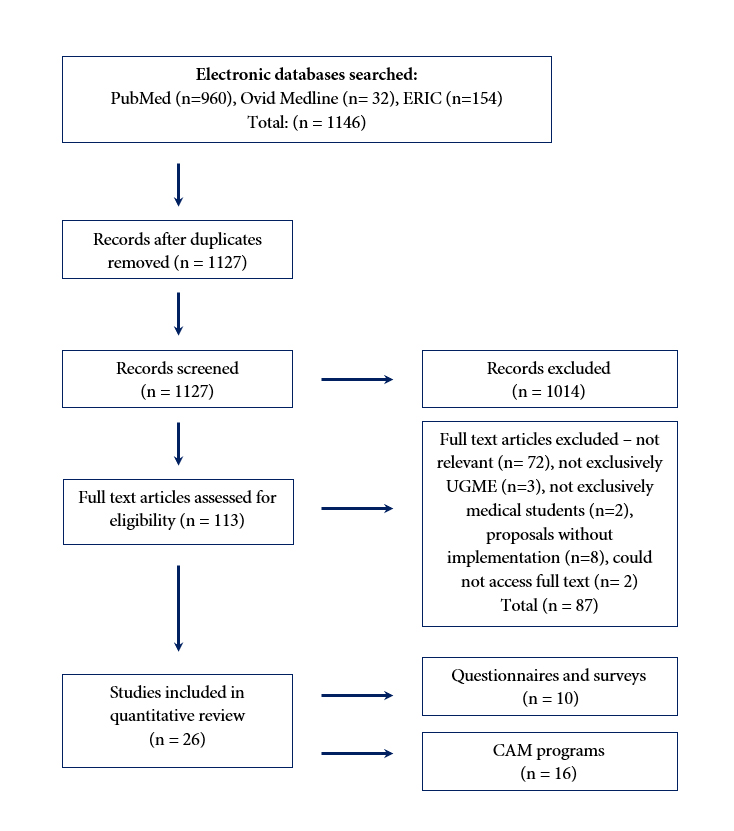
The primary search, which was conducted between July-September 2020, yielded 1146 citations - 960 citations from PubMed, 32 from Medline and 154 from ERIC. After the removal of duplicate citations and those not written in English, 1127 remained. Following a review of titles and abstracts, 113 full-text articles remained, of which 26 met the inclusion criteria. See Figure 1 for the complete search and study selection strategy. A summary of the included studies is found in Table 2 and Table 3. Two main categories of literature were identified: 1. those reporting whether CAM was included in a medical school’s UGME curricula, and; 2. those describing the teaching, learning and assessment approaches implemented in UGME.
Is CAM Being Taught in UGME?
Ten studies directly addressed the inclusion of CAM in UGME curricula (see Table 2). Seven studies9-15 utilised written questionnaires or surveys to collect program information, whilst two16, 17 used a telephone interview, and one 18 used a combination of both. Sampson and Colleagues13 and Brokaw and Colleagues10 assessed CAM education in U.S. medical schools. Sampson and Colleagues reported 45% (56/125) of medical schools offered some form of CAM education. Brokaw and Colleagues reported of 53 U.S medical schools surveyed, 75.3% (40/53) taught an elective CAM course, and 30.1% (16/53) taught a required course, with several schools (7/53) offering both. In neighbouring regions of North America, Ruedy and Colleagues17 found of the 16 Canadian medical schools evaluated, 81% (13/16) reported the inclusion of CAM in their medical programs, and the remaining 19% (3/16) were planning to include CAM teaching in the future. Rampes and Colleagues12 survey of British medical schools reported only 3 of 24 schools (12.5%) offered CAM teaching, and none provided practical training. Smith14 found CAM was included in the curricula of all 18 responding UK medical schools (58% response rate), with 33.3% (6/18) indicating it was taught formally within the UGME curriculum.
In Europe, Brinkhaus and Colleagues 9 surveyed 487 department directors at medical schools in Austria, Germany and Switzerland. Of these, 34% (162/487) indicated CAM had been integrated into their medical schools’ curricula. There was noted inter-country variability with lower CAM integration in Switzerland (20%) compared to Austria (28%) and Germany (27%). Varga and Colleagues15 surveyed 265 medical faculties in European medical schools, reporting that 40% of responding universities offer some form of CAM teaching. In Japan, Tsuruoka and Colleagues18 reported CAM teaching was included in 16 of 80 (20%) schools, with 19 different teaching and learning approaches described. Kim and Colleagues (2012) reported CAM was taught at 85.4% (35/41) of participating Korean medical schools.11 Chitindingu and Colleagues16 survey of seven South African schools reported one school was teaching both Traditional Medicine (T.M.) and CAM, five were teaching either T.M. or CAM, and one was teaching neither. T.M. relates to therapeutic practices that incorporate plant, animal and mineral-based medicines, spiritual therapies, manual techniques and exercises, often practiced in developing countries.19 Whilst TM is regarded as distinct from CAM, TM practices may be included within CAM.20
Data on what elements of CAM are taught in UGME was inconsistently reported. In general, of studies that looked at whether CAM was taught in UGME, acupuncture was the most frequently taught modality11,12,17,18 followed by homeopathy10-12,17 and manipulation or chiropractic therapies.10,12 In studies evaluating how implemented CAM programs are taught, the most commonly taught or demonstrated CAM disciplines were acupuncture21-25 manipulation/chiropractic 24,26, 27 and massage.21-23 Less frequently taught therapies included biofeedback21,26 nutrition21,28 analysis of medicinal plants24 homeopathy26,27 hypnosis26 and osteopathy.27 Several of the identified programs taught about the evidence base of CAM alongside the risks and benefits or offered an opportunity for scientifically evaluating CAM efficacy.21,24,27, 29-32
How is CAM Taught in UGME?
Sixteen articles21-30,32-37 described specific CAM teaching, learning, and assessment approaches in UGME curricula. A detailed breakdown of the different approaches used is described in Table 3. The structure of teaching modules varied greatly between programs. In a unique approach, Da Silva and Colleagues22 reported a split teaching program, where students attended CAM classes in their third year, followed by clinical placements in their fifth year. Meanwhile, other programs included integrated CAM teaching across three 28 four 24, 34 five30 and six years25 of their UGME programs. Other programs adopted a block approach, where teaching was delivered over a period of weeks to months.27-29, 31, 35, 36
Teaching time also varied greatly across institutions. Duration of time ranged from a relatively brief 5 hours21, to the longest of 90 hours.25 Several of the programs with integrated teaching across several years did not report on the total teaching time, including Frenkel and Colleagues34 and Perlman and Stagnaro.24 The teaching modalities used in the delivery of CAM education varied widely. Only one program24 used a solely didactic approach. Others used a didactic approach in conjunction with some form of interactive teachings such as tutorials24, 30 hands-on practice23 discussion-based learning 31,35,36 workshop34 case and team-based learning28 or student-led presentations.35 In a commonly utilised approach, several programs included a clinical placement in combination with formal lectures or tutorials.22,25-28,31 These placements varied in length from one day26 to four-afternoon sessions of unspecified duration22 to 30 hours.25 Bailey and Colleagues21 reported a unique approach involving a seminar followed by an Integrative Medicine fair where over 30 providers interacted with students through a series of student-selected workshops that introduced fields such as nutrition, massage, acupuncture, yoga and biofeedback. Similarly, the program described by Lehmann and Colleagues35 offered a unique one-day excursion to the European Library for Homeopathy (Kothen, Germany).
Generally, the instructors delivering CAM programs were either faculty members of the medical school or clinicians29,30,34-36 external CAM practitioners only26,31 or both.21,24, 25,27,32 Several programs also included visiting experts and scholars from other universities.24,28 In some instances, faculty members were noted to have undergone advanced CAM training.24,32 Several programs involved qualified community or student CAM providers and practitioners, including those with an element of clinical placement.21,23,26,27,31 Post course student evaluations were infrequently used to assess student experiences and overall course satisfaction.26,31 Objective assessment of knowledge and learning was not performed. Where knowledge assessment was completed, it often entailed subjective self-reporting using a Likert scale or other quantitative measure.22,23,27-29,36 Few programs used appropriately coded and thematically interpreted qualitative measures.34,35 Several programs did not have formal evaluative or assessment processes in place24,25,30,37 or removed the evaluative process following a period of time.21
Assessment of Education and Learning Outcomes
This review assessed the educational and learning outcomes of the aforementioned studies using Kirkpatrick’s Hierarchy (Table 2).5-7 There was a clear trend toward Level 1 outcomes, where student reaction and satisfaction were measured in all programs, bar one34 using a post-course evaluation. Likewise, a majority of programs achieved Level 2 outcomes by considering the achievement of learning outcomes by students who completed self-evaluations.21,22,27-29,32,34-36 Only Frenkel and Colleagues34 achieved Level 3 outcomes, where students were asked if and how learned knowledge from the CAM program would change their behaviour. It should be noted behavioural changes were self-reported and not directly observed or analysed. Level 4 outcomes were not achieved by any of the UGME programs included in this review.
Discussion
This scoping review of CAM education in UGME demonstrates the emerging interest in this area. In view of the rising use of CAM and the potential for CAM-conventional therapy interactions, there is an increasing need for physicians to become familiar with common CAM therapies.38 As reported, past and current inclusion of CAM teaching, even within schools located in the same country, is inconsistent. In curricula that include CAM, teaching and learning vary widely, both in terms of content and delivery. It appears agreed statements on the expected skills and competencies of medical students at graduation related to CAM therapies are yet to emerge. In the absence of this consensus, it is difficult to identify clear aims and objectives of any CAM teaching program within a medical course. The following discussion amalgamates the key findings and addresses their implications, with the overall aim of aiding in the development of consistent and equitable medical education.
Program Format and Design
The duration of teaching is one of the greatest areas of inconsistency amongst the included programs. Whilst a number had integrated CAM teaching across one or several years of their curriculum, the design of others was relatively brief, with few - or unspecified - dedicated teaching hours.21,32,37 Meanwhile, several ‘integrated’ programs regarded the practices of mindfulness and self-care for students as an element of their holistic CAM curriculum.23,30 Other medical schools considered mentioning CAM in areas of relevance - such as drug interactions and clinical oncology - constituted sufficient CAM teaching.14 This could lead to a potentially inflated and inaccurate measure of the duration of CAM teaching, particularly within these integrated approaches.
In analysing the approach to teaching, it is clear experiential learning is favoured compared to a solely didactic approach. Nearly all programs favoured delivery methods that would enhance student engagement. These included tutorials, workshops and case discussions, alongside clinical placements with CAM practitioners. Whilst well received by students, most immersive methods only achieved Kirkpatrick’s Level 1 and/or 2 outcomes, without an assessment of translatability to clinical practice and impacts on patient outcomes, which would require Level 3 and 4 outcomes, respectively. Various programs included clinical placements with CAM practitioners, the longest being 30 hours.25 However, in the absence of a student evaluation or objective assessment tool, the benefits of clinical placement cannot be commented on.
Various programs focussed on specific CAM disciplines, the most common of which was acupuncture.21-25 This reflects the identified difficulties in establishing a discrete knowledge base, as CAM disciplines require constant updating as new evidence and novel therapies emerge and gain traction within the general population.3 In what proved to be a popular approach21,24,27,29-32 analysis of the evidence base surrounding CAM is one of the more common methods of teaching. In equipping students with the skill set needed to critically appraise evidence, the plethora of CAM therapies need not be delved into individually. Rather, students can draw their own informed conclusions without the influence of potentially biased and unsubstantiated claims. Despite this, not all programs included teaching on evidence-based medicine (EBM), rather focusing on specific CAM disciplines. In designing a sustainable CAM program, curriculum developers should consider the need for constant review and critical appraisal as new evidence emerges. The EBM teaching model presents a potential solution to a rather overwhelming and resource intensive area of education, where learned knowledge and skills can be adapted for differing CAM modalities, and beyond.
Likewise, the qualifications of CAM educators for such programs must be consistent and their repeated involvement sustainable. Whilst many programs utilised community-based CAM practitioners25,26,31,35 difficulties in repeatedly sourcing appropriately qualified instructors were identified.21 Where faculty staff were involved in teaching, several programs were sustainable for longer.21,22,30 Whilst both CAM practitioners and faculty staff could both introduce an element of bias, this could be overcome with clear learning outcomes and an evidence-based teaching approach. In view of sustainability, it may be more appropriate to deliver teaching through faculty staff, some of who receive further training in EBM. Curriculum developers should consider and account for the additional cost of incorporating CAM programs within UGME.
Appropriate assessment and educational outcomes
Few of the programs performed formalised pre and/or post-course student assessment or evaluation as a measure of the change in knowledge. This reaffirmed findings from Stratton and Colleagues3 which reported the same observation in the programs receiving CAM education grants from the NCCAM. Instead, general qualitative statements were regarded as a measure of overall student satisfaction and increased knowledge.21,27,34 Student reactions and knowledge (Kirkpatrick’s Level 1, 2a, 2b) were the most commonly achieved outcomes, with student knowledge measured subjectively through student questionnaires.22,27-29,31,32 Whilst Frenkel and Colleagues34 was successful in determining the willingness of learners to apply new knowledge and skills (Kirkpatrick’s’ Level 3 outcome), it was the only study to do so. Course designers within medical schools must create educational programs that aim to directly impact patient care, rather than increasing knowledge without a foreseeable change to clinical practice. This is an undoubtedly challenging task, particularly since many widely taught CAM therapies have not yet been proven efficacious by scientific standards. For medical educators to educate appropriately, an evidence base for positive patient outcomes must first be established.
Limitations
Articles may have been omitted due to the adopted search strategy, inclusion criteria, and limit of English language articles only. Grey literature was not performed. Several programs were incompletely reported, potentially influencing the outcomes reported in this review. Many medical school faculty and Deans who were approached did not participate, leading to potential selection bias. Studies incorporating face-to-face interviewing may also be subject to observation bias. A small sample size, apparent in several studies, could also reduce the power and, therefore, reliability of results. Post-evaluations using subjective qualitative Likert-based assessment do not provide an objective measure of program success, particularly where students’ results cannot be compared to pre-program standards. As only the first three levels of Kirkpatrick’s Hierarchy were reached, the patient implications of CAM in UGME could not be determined. No studies reported on the change in patient outcomes or healthcare delivery (Kirkpatrick’s Level 4). Longitudinal prospective studies would provide curriculum developers with insight to the real-world effects of CAM education, where patient outcomes can be correlated to teaching interventions. Several studies did not report outcomes of interest, such as teaching duration, disciplines and teaching staff.22, 27, 28, 31, 32, 37
Conclusions
The aim of this review was to evaluate the various approaches for teaching CAM in UGME. Despite various limitations, it is apparent CAM teaching is inconsistently incorporated into medical schools at a multi-national level. The diversity in approaches reflects the lack of defined graduate competencies as they relate to this specific area. With a breadth of CAM disciplines and an array of teaching and learning approaches, there is no single recommended education program that has been demonstrated to produce positive patient outcomes. Although the concept of an EBM course appeals as a potential solution to overcoming the enormous breadth and content developments in CAM, ultimately there is a deficiency of evidence to demonstrate the real-life healthcare impact. Curriculum developers would be better guided with further research, aligning health outcomes with teaching, assessment and evaluation of proposed CAM programs.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- National Centre for Complementary and Integrative Health. Complementary, alternative, or integrative health: What’s in a name? 2018. [Cited 21 July 2020]; Available from: https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name.
- Yamey G. Can complementary medicine be evidence-based? West J Med. 2000; 173: 4-5.
Full Text PubMed - Stratton TD, Benn RK, Lie DA, Zeller JM and Nedrow AR. Evaluating CAM education in health professions programs. Acad Med. 2007; 82: 956-961.
Full Text PubMed - Quartey NK, Ma PH, Chung VC and Griffiths SM. Complementary and alternative medicine education for medical profession: systematic review. Evid Based Complement Alternat Med. 2012; 2012: 656812.
Full Text PubMed - Bates R. A critical analysis of evaluation practice: the Kirkpatrick model and the principle of beneficence. Evaluation and Program Planning. 2004; 27: 341-347.
Full Text - Kirkpatrick DL, Kirkpatrick JD. Kirkpatrick’s four levels of training evaluation. Alexandria, VA: ATD Press; 2016.
- Ragsdale JW, Berry A, Gibson JW, Herber-Valdez CR, Germain LJ and Engle DL. Evaluating the effectiveness of undergraduate clinical education programs. Med Educ Online. 2020; 25: 1757883.
Full Text PubMed - Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö and Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018; 169: 467-473.
Full Text PubMed - Brinkhaus B, Witt CM, Jena S, Bockelbrink A, Ortiz M and Willich SN. Integration of complementary and alternative medicine into medical schools in Austria, Germany and Switzerland--results of a cross-sectional study. Wien Med Wochenschr. 2011; 161: 32-43.
Full Text PubMed - Brokaw JJ, Tunnicliff G, Raess BU and Saxon DW. The teaching of complementary and alternative medicine in U.S. medical schools: a survey of course directors. Acad Med. 2002; 77: 876-881.
Full Text PubMed - Kim DY, Park WB, Kang HC, Kim MJ, Park KH, Min BI, Suh DJ, Lee HW, Jung SP, Chun M and Lee SN. Complementary and alternative medicine in the undergraduate medical curriculum: a survey of Korean medical schools. J Altern Complement Med. 2012; 18: 870-874.
Full Text PubMed - Rampes H, Sharples F, Maragh S and Fisher P. Introducing complementary medicine into the medical curriculum. J R Soc Med. 1997; 90: 19-22.
Full Text PubMed - Sampson W. The need for educational reform in teaching about alternative therapies. Acad Med. 2001; 76: 248-250.
Full Text PubMed - Smith KR. Factors influencing the inclusion of complementary and alternative medicine (CAM) in undergraduate medical education. BMJ Open. 2011; 1: 000074.
Full Text PubMed - Varga O, Márton S and Molnár P. Status of complementary and alternative medicine in European medical schools. Forsch Komplementmed. 2006; 13: 41-45.
Full Text PubMed - Chitindingu E, George G and Gow J. A review of the integration of traditional, complementary and alternative medicine into the curriculum of South African medical schools. BMC Med Educ. 2014; 14: 40.
Full Text PubMed - Ruedy J, Kaufman DM and MacLeod H. Alternative and complementary medicine in Canadian medical schools: a survey. CMAJ. 1999; 160: 816-817.
PubMed - Tsuruoka K, Tsuruoka Y and Kajii E. Complementary medicine education in Japanese medical schools: a survey. Complement Ther Med. 2001; 9: 28-33.
Full Text PubMed - World Health Organization. Factsheet 134: Traditional Medicine. 2013. [Cited 23 July 2020]; Available from: https://apps.who.int/gb/ebwha/pdf_files/EB134/B134_24-en.pdf.
- Hollenberg D, Zakus D, Cook T and Xu XW. Re-positioning the role of traditional, complementary and alternative medicine as essential health knowledge in global health: do they still have a role to play? World Health Popul. 2008; 10: 62-75.
PubMed - Bailey ML, Chudgar SM, Engle DL, Moon SD, Grochowski CO and Clay AS. The impact of a mandatory immersion curriculum in integrative medicine for graduating medical students. Explore (NY). 2015; 11: 394-400.
Full Text PubMed - da Silva JB, Saidah R, Megid CB and Ramos NA. Teaching acupuncture to medical students: the experience of Rio Preto Medical School (FAMERP), Brazil. Acupunct Med. 2013; 31: 305-308.
Full Text PubMed - Hoffmann DS, Dancing D and Rosenbaum M. Massage and medicine: an interprofessional approach to learning musculoskeletal anatomy and enhancing personal wellness. Acad Med. 2019; 94: 885-892.
Full Text PubMed - Perlman A and Stagnaro-Green A. Developing a complementary, alternative, and integrative medicine course: one medical school's experience. J Altern Complement Med. 2010; 16: 601-605.
Full Text PubMed - Tahzib F and Daniel SO. Traditional medicine and the modern medical curriculum. Lancet. 1986; 2: 203-204.
Full Text PubMed - Laken MP and Cosovic S. Introducing alternative/complementary healing to allopathic medical students. J Altern Complement Med. 1995; 1: 93-98.
Full Text PubMed - Owen D and Lewith GT. Complementary and alternative medicine (CAM) in the undergraduate medical curriculum: the Southampton experience. Med Educ. 2001; 35: 73-77.
Full Text PubMed - Karpa K. Development and implementation of an herbal and natural product elective in undergraduate medical education. BMC Complement Altern Med. 2012; 12: 57.
Full Text PubMed - Forjuoh SN, Rascoe TG, Symm B and Edwards JC. Teaching medical students complementary and alternative medicine using evidence-based principles. J Altern Complement Med. 2003; 9: 429-439.
Full Text PubMed - Hassed CS. Bringing holism into mainstream biomedical education. J Altern Complement Med. 2004; 10: 405-407.
Full Text PubMed - Jeffries WB. A fourth-year elective course in alternative medicine. Acad Med. 2001; 76: 525-526.
Full Text PubMed - Mahapatra S, Bhagra A, Fekadu B, Li Z, Bauer BA and Wahner-Roedler DL. Incorporation of integrative medicine education into undergraduate medical education: a longitudinal study. J Integr Med. 2017; 15: 442-449.
Full Text PubMed - Hasler DLME and Leggit JC. Complementary and integrative health education in the medical school curriculum: an interest survey. Med Acupunct. 2018; 30: 298-307.
Full Text PubMed - Frenkel M, Frye A, Heliker D, Finkle T, Yzaguirre D, Bulik R and Sierpina V. Lessons learned from complementary and integrative medicine curriculum change in a medical school. Med Educ. 2007; 41: 205-213.
Full Text PubMed - Lehmann B, Krémer B, Werwick K and Herrmann M. Homeopathy as elective in undergraduate medical education--an opportunity for teaching professional core skills. GMS Z Med Ausbild. 2014; 31: 7.
Full Text PubMed - Ma X, Xu B, Liu Q, Zhang Y, Xiong H and Li Y. Effectiveness of evidence-based medicine training for undergraduate students at a Chinese Military Medical University: a self-controlled trial. BMC Med Educ. 2014; 14: 133.
Full Text PubMed - Maharaj SR. Preparing medical graduates to practise in a changing environment: complementary/alternative medicine in the medical undergraduate curriculum of the University of the West Indies. West Indian Med J. 2010; 59: 284-286.
PubMed - Akinola OB. Should complementary and alternative medicine familiarisation modules be taught in African medical schools? Zhong Xi Yi Jie He Xue Bao. 2011; 9: 1165-1169.
Full Text PubMed