Evaluation of online interprofessional simulation workshops for obstetric and neonatal emergencies
Namrata Prasad1, Shavi Fernando1, Sue Willey2, Kym Davey2, Jennifer Hocking3, Atul Malhotra4 and Arunaz Kumar1
1Department of Obstetrics and Gynaecology, Monash University, Melbourne, Australia
2Monash Nursing and Midwifery, Monash University, Melbourne, Australia
3School of Nursing, Midwifery and Paramedicine, Australian Catholic University, Melbourne, Australia
4Department of Paediatrics, Monash University, Melbourne, Australia
Submitted: 11/03/2022; Accepted: 09/10/2022; Published: 31/10/2022
Int J Med Educ. 2022; 13:287-304; doi: 10.5116/ijme.6342.9214
© 2022 Namrata Prasad et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution License which permits unrestricted use of work provided the original work is properly cited. http://creativecommons.org/licenses/by/3.0
Abstract
Objectives: To explore student perceptions of learning and interprofessional aspects of obstetric and neonatal emergencies through online simulation-based workshops.
Methods: This qualitative study was conducted at Monash University, Australia. Data were obtained from six separate online Obstetric Neonatal Emergency Simulation workshops held between May 2020 and August 2021. A total of 385 students attended and were invited to participate in the study by completing an online survey two-three weeks later. Of the attendees, 144 students completed the survey (95 medical, 45 midwifery), equating to a response rate of 37%. Survey responses were downloaded from online survey platform and separated into medical and midwifery responses. Thematic analysis of data was performed using a coding framework, resulting in development of themes and subthemes.
Results: Main themes were adaptability, connectivism, preparedness for practice, experiential learning, learning through modelling and dynamics of online interaction. Students reported that online workshop was a useful alternative method to experience simulation-based learning, increase their readiness for clinical practice and foster positive interprofessional relationships. Consistent with existing literature evaluating similar in-person programs, midwifery students were most interested in interprofessional interaction (predominant theme: dynamics of online interaction), whilst medical students were more concerned with developing clinical skills (predominant themes: learning through modelling, experiential learning).
Conclusions: Online learning may be a useful and convenient way of delivering interprofessional simulation-based education during the pandemic, in remote areas and as an adjunct to in-person teaching. Future studies should evaluate the impact of online learning with a mixed methods study and in comparison, to in-person programs.
Introduction
The development of clinical skills during training years is essential in establishing a competent, safe and efficient healthcare workforce.1 In obstetrics and gynaecology, clinical skills education has been demonstrated to improve patient outcomes and satisfaction.2 Simulation-based education (SBE) and interprofessional education (IPE) have emerged as effective methods of team-based clinical learning.2
In the context of obstetric emergencies, combining IPE and SBE is ideal due to the involvement of a multidisciplinary team in their management and the high-risk nature and rarity of such situations in real life. A program that incorporates aspects of both IPE and SBE is the Obstetric and Neonatal Emergency Simulation (ONE-Sim) workshop.3,4 This workshop simulates obstetric and neonatal emergencies, aiming to improve situational awareness, preparedness for practice, interprofessional communication and teamwork between medical and midwifery disciplines.
The novel coronavirus (COVID-19) pandemic resulted in a shift in all forms of interactions, including in social5 and educational contexts. Throughout the pandemic, there has been increased uptake of social networking and video conferencing platforms in order to maintain a sense of connectedness.5 Across universities, video conferencing has been used as an alternative platform to deliver teaching that has traditionally been in-person, such as small group sessions and tutorials. At our university, the ONE-Sim workshops were also transitioned to an online format, and we published our initial experience using this format in 2020.4
In light of the ongoing COVID pandemic, there is a growing body of literature evaluating SBE delivered in an e-learning format.6-8 These studies demonstrate online SBE is able to achieve high levels of student satisfaction, concept understanding and psychomotor skill development whilst acknowledging limitations of online simulation, such as technical feasibility, particularly in low and middle-income countries where technological resources are potentially fewer, and logistical issues.7 Similarly, since the onset of the pandemic, multiple studies have evaluated online IPE programs in healthcare. These studies demonstrate IPE delivered in online settings is able to help foster positive attitudes towards teamwork, interprofessional communication and collaboration. Students also felt that learning through online IPE could improve outcomes for their patients.9-11
With ongoing recommendations for social distancing where possible in many countries, the need for effective online teaching alternatives remains. Although in-person SBE has long formed an integral part of obstetric training and education and has been heavily appraised in the literature,12 there is a scarcity of studies evaluating online SBE in obstetrics. Moreover, although there is increasing evidence supporting the use of online IPE and SBE programs individually, there are very few studies evaluating a combined online IPE and SBE program. Evaluation of such programs is particularly important in the field of obstetrics, where combining IPE and SBE is ideal due to the multidisciplinary, high-stakes nature of the specialty. Finally, whilst the existing literature evaluates learning outcomes from online SBE or IPE programs, there is a limited exploration of the influence of the online setting on pedagogies.
Our study aims to address this gap in the literature by evaluating an online combined SBE and IPE program specific to obstetric training from the perspective of medical and midwifery students to answer the following research questions:
1. How do students perceive learning in the novel online format?
2. What are students’ perceptions of obstetric and neonatal emergencies when observed through online simulation?
3. How do medical and midwifery students perceive the interprofessional aspects of management of these emergencies when delivered online?
Methods
Study design and participants
An inductive qualitative research design based on post-workshop survey data was employed. The study population consisted of all fourth-year medical students at Monash University on their Obstetrics and Gynaecology rotation (n=250 per year), and midwifery students from Monash University (n=49 per year) and Australian Catholic University (n=60, only invited to 2021 workshops). These students were invited by email to attend one of the six online ONE-Sim workshops held between May 2020 and August 2021 and to subsequently complete a post-workshop survey. A total of 385 students (269 medical, 116 midwifery) attended one of the six online ONE-Sim workshops between May 2020- August 2021.
Given the study was based on a novel initiative where students participated in online obstetric and neonatal simulation, the study participants’ experiences would be highly specific. The sample, therefore, consists of participants with dense specificity, enhancing the information power of the data.
Students were included in our study if they attended one of the online ONE-Sim workshops, consented to study participation and completed the post-workshop survey. Of the 385 students who had attended one of the six online workshops, 144 students (95 medical, 49 midwifery) participated in the study, equating to a response rate of 37%. The low response rate is likely attributable to the delay between students attending the workshop and the post-workshop survey being sent to students. We had designed the study such that the survey would be sent 2-3 weeks after attending the workshop, so that students had the opportunity to reflect on their learning from the workshop and the interprofessional interactions they observed. However, as a result, students’ motivation to complete an optional survey a few weeks after attending the workshop may have been reduced.
Low risk ethics approval for this study was obtained from the Monash University Human Research Ethics Committee. A consent form and explanatory statement detailing study information were attached to the email inviting the study population to attend the online workshop. The consent form clearly documented that study participants were free to withdraw consent at any time during the project without affecting their academic progression or assessments.
Survey
The survey questions are listed in the Appendix. The survey consisted of four open-ended “free text” questions aimed to address the study objectives and questions relating to demographic information such as age, gender and professional group (medical or midwifery). The surveys were drafted by the medical and midwifery educators on the research team and later reviewed by faculty members and students (who did not participate in the study) for validation. The process involved multiple rounds of review and was carried over a duration of 3 months. Free text questions were chosen to get thick descriptions of how students perceived learning by observation of simulation scenarios. To evaluate students’ perceptions of learning in an online format, we developed a question exploring how learning via video conferencing will influence students’ future clinical practice. To understand how students perceive obstetric and neonatal emergencies when observed online, we developed questions comparing students’ experience of in-person obstetrics teaching with the online workshop. To explore students’ perceptions of the interprofessional aspects of obstetric and neonatal emergencies in an online setting, we developed questions pertaining to their experiences of interacting with other professional groups online and whether they would prefer intra-disciplinary to interprofessional teaching when delivered online. In the study, both the research and survey questions were quite specific. Hence, it was anticipated that there would be sufficient information power to provide rigor to the study.
Data collection
Across six independent workshops held between May 2020 and August 2021, a total of 95 medical and 49 midwifery students participated in the study (n = 144). Study participants completed an online survey via “Qualtrics” (Qualtrics, Provo, UT), sent to their student email IDs by the ONE-Sim administrative staff 2-3 weeks after completing the online ONE-Sim workshop. The survey was sent at this time point so that students had the opportunity to reflect on their learning from the workshop and the interprofessional interactions they observed. Students were informed that all responses would be anonymous. NP was given access to the survey responses on Qualtrics, and downloaded and collated responses into an Excel spreadsheet verbatim. Since participants were made aware that survey responses were anonymous and had no effect on their academic assessment, they would likely feel more comfortable expressing their true thoughts and feelings in the survey responses. In combination with relatively specific survey questions, the quality of dialogue is strong, ensuring sufficient information power. Credibility was ensured through data and investigator triangulation. Data was triangulated by using survey responses relating to six separate workshops held at different time points between May 2020 and August 2021. Investigator triangulation was achieved through two different investigators independently performing analysis of the data and multiple different researchers reviewing the final themes yielded from thematic analysis.
Study setting
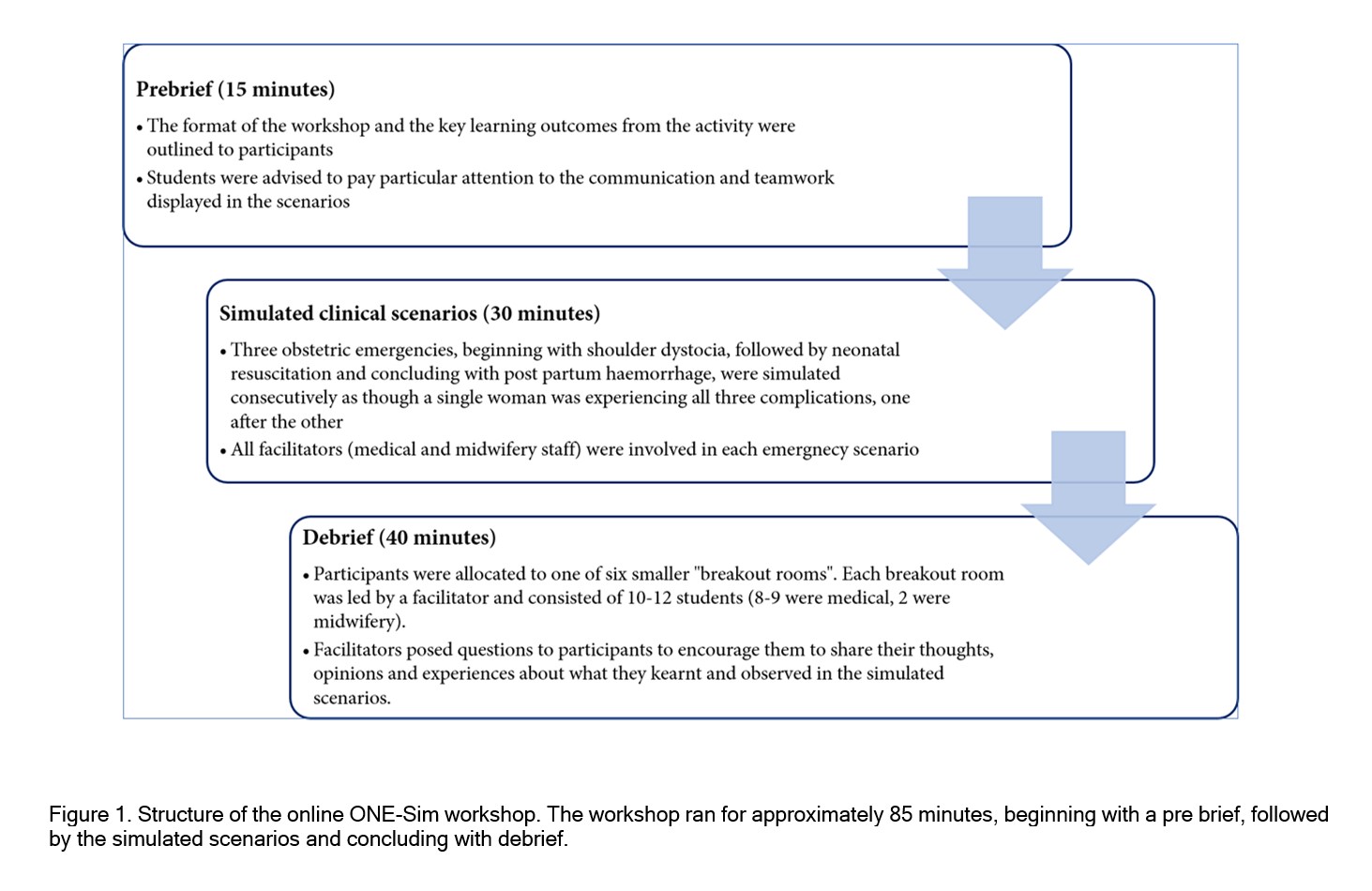
The study was performed at Monash University, Australia. The online ONE-Sim program has been described in detail previously.4 In brief, the workshop was conducted online via a video conferencing platform, “Zoom”. The workshop was approximately 85 minutes in duration. The structure of the workshop is outlined in Figure 1 and includes a pre-brief followed by simulation scenarios and ending with a de-brief.
At the time of attending the online ONE-Sim, both medical and midwifery students were undergoing clinical placements in the birth suites of various affiliated hospitals. However, due to differences in course length and structure, medical students had completed less than 12 weeks of clinical placement, whereas midwifery students had a longer stint in clinical placements. Due to pandemic restrictions, both groups had received limited structured or large-group in-person learning in the preceding months.
Analysis methods
Within the Excel spreadsheet, data were separated into medical and midwifery student responses. Thematic analysis was performed on each set of survey responses. A coding framework was first created.13 NP and AK inductively and independently coded the survey responses. The qualitative dataset was found to be comprehensive enough to identify recurring codes and patterns to generate adequate information power. A set of themes was independently developed from these codes. AK and NP then agreed upon these themes, closely reflecting participants’ own responses. The second phase of the analysis involved identifying subthemes nested within each higher-order theme. The third phase involved negotiation, discussion and collective review of data by NP, AK and other co-investigators JH, SW, KD, SF and AM to yield final themes.
Results
Thematic analysis
Major themes and sub-themes are described below in the order of what was considered most dominant by both groups (Table 1), the medical group (Table 2) and the midwifery group (Table 3). Common themes between the groups related to “adaptability”, “connectivism” and “preparedness for practice”. The predominant themes identified in medical student evaluations were “experiential learning” and “learning through modelling”. The major theme predominantly identified in midwifery students was “dynamics of online interaction”.
Adaptability
The COVID-19 pandemic and the requirement to socially distance represent circumstances outside the student's control. Adaptability is related to students’ capacity to cope with a lack of in-person teaching and learning through an alternate delivery of teaching, e-learning, with which they may be less familiar. The subthemes within this main theme were “comfort with e-learning”, “responding to dynamic circumstances”, and “future applications of e-learning”; e.g., “I thought given we couldn’t be there in person, nor practice our potential future role in the scenario, the Zoom session was an excellent alternative.”; “I think that this was beneficial …as we have done a lot of simulation …so this was a good opportunity to consolidate our knowledge in a different way, through reflection.” (MED 12, Table 1).
Connectivism
Connectivism is the concept of digital technologies, such as the video conferencing platform employed in this study, providing new avenues for learning. Specifically, learning exists as a “network” of learners (in this study, midwifery and medical students) who are influenced by technology and social interactions. The subthemes within this main theme are “facilitators as nodes in the learning network” and “diversity of opinions”; e.g., “Through interacting with different professions and educators, I feel that it was an eye-opening experience.” (MW 4, Table 1); “I found it eye-opening to have a workshop alongside the midwifery students. They have a lot of input and suggestions when it came to the content. I got to ‘see’ what are the thoughts in their minds during an emergency situation.” (MED 34, Table 1).
Preparedness for practice
“Preparedness for practice” revolves around the simulation’s ability to increase student confidence in approaching clinical situations in work-based placement. The theme explored greater awareness of their own role in a clinical setting, both as a student currently and their projected role as a qualified practitioner, as a result of the simulation. Additionally, it encompassed the interprofessional rapport and relationships formed through exposure to and interaction with students from other disciplines as part of the program. The subthemes within this main theme were “role self-awareness within a team, both as a student and in their projected role” and “fostering positive working relationships at a grassroots level that will be reflected in future practice”; e.g., “…fostering mutual respect at a student level is a real positive” (MW 18, Table 1); “I think I have better insight into how to navigate my role in an emergency, which will definitely be important in my future practice” (MED 89, Table 1).
Experiential learning
Experiential learning refers to the real-time, hands-on aspects of simulation-based education and the fidelity of the simulation to real-world scenarios. The main theme of experiential learning was divided into further subthemes relating to the “personal stress response to real-time emergencies” associated with enacting a simulated emergency oneself, as well as “learning by doing”, where students are referring to the practical experience of developing core skills through the workshop. Additional subthemes within this main theme were, “lack of physical interaction”, “clinical skills confidence” and “creating realism through e-learning”; e.g., “It was a bit difficult to learn this over zoom, especially because we didn’t have the opportunity to be hands on” (MED 1, Table 2); “…that lack of adrenaline means a valuable facet was lost from the demonstration” (MED 32, Table 2).
Learning through modelling
“Learning through modelling” captured the experience of students observing expert healthcare professionals partake in the simulation, who was setting a “standard of care” or displaying ideal practice. The behaviours, actions and interactions between team members demonstrated in the simulation form a “model” that students can then emulate in the workplace when they are qualified practitioners themselves. The subthemes within this main theme are “perceiving individual’s projected roles”, “interpersonal interactions”, “intrapersonal emotional regulation” and “patient-centredness”; e.g., “I learnt how a well-drilled team makes management of an emergency flow smoothly…” (MED 12, Table 2); “…the environment in an obstetric emergency can rapidly degenerate into one of panic…we need to be extremely proficient … so we can collect ourselves and respond adequately” (MED 39, Table 2).
Dynamics of online interaction
This theme represents the interplay between medical and midwifery students and how the online setting of the workshop impacted both their communication with one another and on a deeper level, their perceptions of one another, including dominance in the discussion, the willingness to participate in interprofessional interactions, and mutual respect and appreciation in the workplace. The subthemes within this main theme are “dominance of a professional group”, “power imbalance relating to their greater knowledge and clinical experience than the medical student”, “equality of opinions”, “contribution from more clinically experienced midwifery students leading to increased learning by medical fraternity” and “awareness of clinical challenges” (Table 3).
Discussion
The study evaluated student learning through online simulation workshops conducted over a 16-month period and found that the key learning outcomes between medical and midwifery students were similar to studies evaluating in-person simulation programs. The main themes arising from the evaluation of the online ONE-Sim workshops overlapped between medical and midwifery student groups but appeared to have a slightly different focus. Midwifery students indicated that they were more interested in interprofessional interactions, fostering positive relationships and a power balance, with the predominant theme being “dynamics of online interaction”. In contrast, medical students were most concerned with “learning through modelling” and “experiential learning”.
Social distancing measures implemented during the COVID-19 pandemic necessitated a transition to online learning. The online workshop format was designed on the concept of “learning through observation”, which has previously been studied.14 The majority of studies demonstrate that learning through observation is equally useful, or in some cases, better than “hands-on” participation in simulation, and is associated with high levels of learner satisfaction. Factors correlated with greater learning and satisfaction in the learning through observation framework include the use of observer tools, learner engagement and active participation in debriefing.14 We ensured these factors were considered when transitioning the ONE-Sim workshop from an in-person to an online format. An example of an observer tool is providing observers with an instructional briefing.14 In our study, this tool was implemented in the form of the “prebrief” (Figure 1) where participants were provided clear instructions on how the simulation would be conducted and particular elements of the simulation to pay attention to. When designing the structure of the online workshop, we ensured that a large proportion of the workshop was devoted to debriefing, an important element of successful "learning through observation” initiatives. Moreover, the majority of discussion within the debrief session was student driven to facilitate participants actively contributing to the debrief.
One of the greatest challenges in transitioning the ONE-Sim workshop to an online format was the familiarisation of facilitators and administrative with technologies such as video recording and video conferencing. Though these technologies have existed for many years, they had not been used as extensively or regularly by educators prior to the pandemic. Specific challenges included ensuring accessibility to the link to the online workshop, camera angles enabled a clear view of the simulation, and facilitators were able to quickly and effectively launch breakout rooms in the debrief. Multiple practices of the simulation and review of the content by study investigators and administrative staff were required prior to the formal commencement of the program. It was observed that most medical students were more task-oriented, whereas midwifery students were more relationship-oriented. This could be due to inherent differences in learning styles. According to Kolb’s learning theory, there are four main learning styles: accommodating, diverging, assimilating and converging.15 Medical students have been shown to most commonly adopt the “assimilator” learning style.16 which is described as a logical approach to learning, where “ideas and concepts are more important than people”.15 By contrast, midwifery students mostly demonstrate a “diverging” learning style.17 described as “sensitive” and more focused on people.15 The predominant learning styles described amongst medical and midwifery students closely reflect the major themes arising in each disciplinary group.
The different learning outcomes from a shared educational experience demonstrated in this study are in keeping with an earlier paper reporting on an in-person IPE program similar in content and structure to the ONE-Sim program.3 The in-person workshop with medical and midwifery students demonstrated “learning by doing” as the key theme in medical students, while the midwifery students focussed around “power” and “roles and relationships”. This is similar to our current study, where key themes from medical students were related to the learning experience and through role modelling while midwifery students were focused on interaction with the medical students. This suggests the remote format of the obstetric interprofessional workshop may not significantly affect the main learning outcomes and patterns of focus between professional groups. Furthermore, it highlights both the strength of the association between profession and key learning areas and the realism to the original in-person simulation able to be achieved through the online format.
The findings also raise the possible difference in the occupation culture that may influence learning patterns in professional groups. Although medical students were in their fourth year of a five-year course, they are still a few years away from being able to practise as independent clinicians till they complete their speciality training; hence, their keenness to gain more procedure-based experience in early clinical learning years. By contrast, midwifery students are further into their clinical practice and have more experience in clinical birth settings. Hence, their focus is on how the interaction between colleagues can affect their future clinical practice. Midwifery students were particularly interested in the dynamics of online interactions. Due to their greater exposure to clinical practice, and discussion surrounding the interprofessional model of care early on in their training, some midwifery students may have drawn upon their own experiences in the workplace and were more aware of the challenges afflicting the doctor-midwife relationship. These were largely pertaining to mutual respect and appreciation for each profession’s skills and knowledge.
Acknowledgement of these challenges in a virtual setting provides evidence that e-learning may influence team-based attitudes and highlights the realism that can be created. Moreover, as was described, based on an in-person simulation program,3 midwifery students use their relative greater clinical and specialized theoretical knowledge and experience compared to medical students to gain respect for their profession and assert their power in the group. While medical and midwifery colleagues work closely together in a birth setting, their philosophy of learning may vary18 and possibly may drive divergent work culture.19 IPE at a student level may perhaps assist in closing this gap.
Both medical and midwifery students also expressed how the experiential learning aspect of the ONE-Sim program differed between the online and in-person formats. Unsurprisingly, both groups felt the online simulation of emergencies was not able to induce the same personal stress response as an in-person workshop potentially could have. This may be because the in-person ONE-Sim required students to perform the scenario themselves, compelling them to make critical decisions, communicate with the multidisciplinary team and carry out tasks under time pressurei20. By contrast, in the online ONE-Sim, students observe rather than partake in actively simulated emergencies and intercede as required, thus taking away the real-time experience and removing the anxiety of making ‘life-threatening’ decisions under time constraints. In effect, by managing the emergency themselves in the in-person workshop, students may have felt more accountable, increasing their own personal stress levels. Regulation of stress levels and greater ability to engage in rapid, accurate decision-making in obstetric emergency settings has been shown to improve neonatal and maternal outcomes.21 Reduced ability to gain experience in these important skills decreases the utility of online simulation programs when specifically addressing knowledge and experiential themes.
Although certain aspects of experiential learning may have been reduced through the online ONE-Sim, both groups, particularly medical students, noted online learning facilitated “learning through modelling”. Learning through modelling is becoming an increasingly recognized framework in healthcare education.22 The concept of a “role model” is founded upon two key theories. First, individuals are able to identify others holding a societal role or position to which they aspire to hold themselves.22 For the study participants, the senior obstetricians and midwives involved in the simulation, represented the roles that medical and midwifery students may have wished to hold themselves in their future practice. Secondly, the theory of social learning, where individuals actively observe role models’ behaviours as they believe this will assist them in learning advantageous skills and social norms in a particular context and adopt these behaviours themselves.22 By observing their chosen role model (obstetrician, neonatologist or midwife) in the simulated online emergencies, students developed greater understanding of the behaviours and demeanours that are expected of them in a professional environment, enabling them to implement these in their own future clinical practice.
Students commented not only on the individual behaviours of their role models but also on the interpersonal interactions occurring on a team level. The team simulating the emergency as a cohesive unit can also be considered a “role model” as students strive to become a member of the future multidisciplinary team. Thus, the communication, teamwork, role delegation and leadership demonstrated in the online workshop sets a standard of care and ideal practice that the students may emulate once they enter the workforce and become a member of an interprofessional team themselves. However, learning through role modelling in a simulation also poses the risk of students adopting poor or non-evidence-based practices that they may observe. Hence, it is important that students get an opportunity for open discussion as part of the learning process to allow different ideas to be heard, so they can identify and emulate best practice. Both groups of students noted the broader applications of online learning. These include greater convenience and reduced travel time compared to in-person teaching sessions, consolidation of previous in-person learning; and improving consistency of clinical exposure. These benefits of online learning have implications for medical education practice beyond the pandemic. Implementation of online SBE and IPE programs may be considered in geographically remote areas where participation in face-to-face teaching may be limited by distance. Moreover, in remote and regional areas, there may be reduced availability of appropriately trained staff to facilitate such programs. The use of online SBE and IPE programs enables centralization of expert facilitators to deliver education to students in various geographical locations.
The results of our study support findings from the existing literature exploring the effectiveness of online learning models amongst healthcare students. As in previous studies,23 participants in our study found online learning a useful means of consolidating and enhancing their clinical skills and knowledge, captured in the theme “preparedness for practice”. In our study, students particularly felt that the debrief session held after the simulation, which enabled students to interact with one another and share ideas, was a useful means of improving communication skills and enhancing teamwork. These findings of improved communication and teamwork skills echo the results of an online program run at Harvard Medical School involving virtual “teams” that aimed to help the community and healthcare system during the pandemic.24 Furthermore, the theme of adaptability that arose in our study, particularly pertaining to the convenience and improved accessibility that online learning affords, has been reported in numerous studies.23 In light of these findings and the existing literature, online SBE and IPE programs may be considered for formal integration in healthcare education to supplement and enhance in-person teaching. Whilst there is a growing body of evidence demonstrating the effectiveness and advantages of online learning, it is important to note the potential adverse effects of online learning on mental illness amongst healthcare students. For example, a recent systematic review demonstrated that whilst the prevalence of anxiety amongst medical students during the pandemic remains similar to pre-pandemic, there are a number of stressors specific to the pandemic and online learning that correlate with higher anxiety levels.25 Online learning has been associated with fear of confinement and impaired ability to progress their education amongst students, contributing to increased levels of anxiety.26 Considering and mitigating these potential adverse effects is essential prior to the formal incorporation of online learning into the curriculum.
Limitations of our study include varying levels of clinical exposure of each group of workshop attendees at different stages of the pandemic. For example, students with greater clinical exposure may find the online ONE-Sim less helpful as they may have already developed or become familiar with the skills demonstrated in the workshop. A further limitation is the relatively low response rate amongst workshop attendees and the optional completion of the survey. Moreover, the majority of study participants had only attended the online ONE-Sim workshop. Therefore, it is difficult to directly compare students’ perceptions and learning from the online format to the in-person workshop. Finally, as our study uses a self-reported survey as the primary means of evaluation of the online workshop, there is a possibility that the findings are limited by both self-assessment and social desirability bias. For example, due to self-assessment bias, students may overestimate their perceived improvement in clinical skills or increased preparedness for practice, thereby overestimating the utility of and learning derived from online simulation workshops. Social desirability bias may particularly limit the findings of the reported experience of online interprofessional interactions through the workshop. For example, a medical student may report only the positives of learning alongside midwifery students without outlining the drawbacks of the interprofessional education, as this may be perceived as a more socially “desirable” or “acceptable” opinion. However, we hope to have minimized the effect of social desirability bias by using an anonymous survey.
Conclusions
E-learning may be a valuable and meaningful way of delivering simulation-based interprofessional education. The study demonstrated that students were still able to achieve many of the learning objectives through the workshop, albeit through alternative learning methods, such as learning through modelling. While the interprofessional learning aspects of the workshop did not appear to suffer as a result of the online delivery format, the learning of actual hands-on procedural skills could not be adequately replaced in an online format.
The findings of our study have multiple implications in the evolving field of medical education. COVID is likely to persist for the foreseeable future, and as a result, there is an ongoing need for remote education alternatives in line with social distancing. Our study demonstrates online SBE and IPE programs are an effective and useful method of improving students’ preparedness for practice, delivering clinical skills education, and developing positive working relationships between professional groups during the pandemic. Beyond the pandemic, online SBE and IPE may be used in geographically remote areas where students may otherwise be required to commute long distances to receive SBE and IPE, or where there may be staffing issues that prevent easy access to SBE and IPE. Finally, online programs incorporating SBE and IPE may be used as an adjunct to in-person programs to enhance student learning and their overall learning experience. To better understand the impact of the online format on student learning, mixed methods study with a comparison to data based on in-person programs should be considered.
Conflict of Interest
The authors declare that they have no conflict of interest.
Supplementary materials
Supplementary file 1
Appendix. The post-workshop survey (S1.pdf, 89 kb)References
- Bäwert A and Holzinger A. Practice makes perfect! Patient safety starts in medical school: do instructional videos improve clinical skills and hygiene procedures in undergraduate medical students? GMS J Med Educ. 2019; 36: 16.
Full Text PubMed - Cass GK, Crofts JF and Draycott TJ. The use of simulation to teach clinical skills in obstetrics. Semin Perinatol. 2011; 35: 68-73.
Full Text PubMed - Kumar A, Wallace EM, East C, McClelland G, Hall H, Leech M, et al. Interprofessional simulation-based education for medical and midwifery students: a qualitative study. Clinical Simulation in Nursing. 2017;13(5):217-27.
- Prasad N, Fernando S, Willey S, Davey K, Kent F, Malhotra A and Kumar A. Online interprofessional simulation for undergraduate health professional students during the COVID-19 pandemic. J Interprof Care. 2020; 34: 706-710.
Full Text PubMed - Bzdok D and Dunbar RIM. The neurobiology of social distance. Trends Cogn Sci. 2020; 24: 717-733.
Full Text PubMed - Badiee F, Kaufman D. Effectiveness of an online simulation for teacher education. Journal of Technology and Teacher Education. 2014;22(2):167-86.
- Díaz-Guio DA, Ríos-Barrientos E, Santillán-Roldan PA, Mora-Martinez S, Díaz-Gómez AS, Martínez-Elizondo JA, Barrientos-Aguiñaga A, Arroyo-Romero MN, Ricardo-Zapata A and Rodríguez-Morales AJ. Online-synchronized clinical simulation: an efficient teaching-learning option for the COVID-19 pandemic time and: beyond. Adv Simul (Lond). 2021; 6: 30.
Full Text PubMed - McCoy CE, Sayegh J, Rahman A, Landgorf M, Anderson C and Lotfipour S. Prospective randomized crossover study of telesimulation versus standard simulation for teaching medical students the management of critically ill patients. AEM Educ Train. 2017; 1: 287-292.
Full Text PubMed - Guraya SY, David LR, Hashir S, Mousa NA, Al Bayatti SW, Hasswan A and Kaouas M. The impact of an online intervention on the medical, dental and health sciences students about interprofessional education; a quasi-experimental study. BMC Med Educ. 2021; 21: 457.
Full Text PubMed - Liller KD, Pruitt Z and Burke SG. Interprofessional education: reaching health professionals with an interactive professional virtual/online event on advocacy and policy. Front Public Health. 2020; 8: 606394.
Full Text PubMed - Singh J and Matthees B. Facilitating interprofessional education in an online environment during the COVID-19 pandemic: a mixed method study. Healthcare (Basel). 2021; 9: 567.
Full Text PubMed - Dillon S. Simulation in obstetrics and gynecology: a review of the past, present, and future. Obstet Gynecol Clin North Am. 2021; 48: 689-703.
Full Text PubMed - Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77-101.
- O'Regan S, Molloy E, Watterson L and Nestel D. Observer roles that optimise learning in healthcare simulation education: a systematic review. Adv Simul (Lond). 2016; 1: 4.
Full Text PubMed - McLeod SA. Kolb - learning styles and experiential learning cycle. 2017; [Cited 12 December 2022]; Available from: https://www.simplypsychology.org/learning-kolb.html.
- Borracci RA and Arribalzaga EB. [Kolb's learning styles in medical students]. Medicina (B Aires). 2015; 75: 73-80.
PubMed - Shirazi F and Heidari S. The relationship between critical thinking skills and learning styles and academic achievement of nursing students. J Nurs Res. 2019; 27: 38.
Full Text PubMed - Kumar A, Sweet L. Obstetric and midwifery education: context and trends. In: Nestel D, Reedy G, McKenna L, Gough S, editors. Clinical education for the health professions: theory and practice. Singapore: Springer Singapore; 2020.
- McCourt C, Rayment J, Rance S, Sandall J. An ethnographic organisational study of alongside midwifery units: a follow-on study from the Birth-place in England programme. Southampton (UK): NIHR Journals Library; 2014.
- Reime MH, Johnsgaard T, Kvam FI, Aarflot M, Engeberg JM, Breivik M and Brattebø G. Learning by viewing versus learning by doing: a comparative study of observer and participant experiences during an interprofessional simulation training. J Interprof Care. 2017; 31: 51-58.
Full Text PubMed - Heller G, Bauer E, Schill S, Thomas T, Louwen F, Wolff F, Misselwitz B, Schmidt S and Veit C. Decision-to-delivery time and perinatal complications in emergency cesarean section. Dtsch Arztebl Int. 2017; 114: 589-596.
Full Text PubMed - Horsburgh J and Ippolito K. A skill to be worked at: using social learning theory to explore the process of learning from role models in clinical settings. BMC Med Educ. 2018; 18: 156.
Full Text PubMed - Wilcha RJ. Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ. 2020; 6: 20963.
Full Text PubMed - Soled D, Goel S, Barry D, Erfani P, Joseph N, Kochis M, Uppal N, Velasquez D, Vora K and Scott KW. Medical student mobilization during a crisis: lessons from a COVID-19 medical student response team. Acad Med. 2020; 95: 1384-1387.
Full Text PubMed - Lasheras I, Gracia-García P, Lipnicki DM, Bueno-Notivol J, López-Antón R, de la Cámara C, Lobo A and Santabárbara J. Prevalence of anxiety in medical students during the COVID-19 pandemic: a rapid systematic review with meta-analysis. Int J Environ Res Public Health. 2020; 17: 6603.
Full Text PubMed - Li HY, Cao H, Leung DYP and Mak YW. The psychological impacts of a COVID-19 outbreak on college students in China: a longitudinal study. Int J Environ Res Public Health. 2020; 17: 3933.
Full Text PubMed